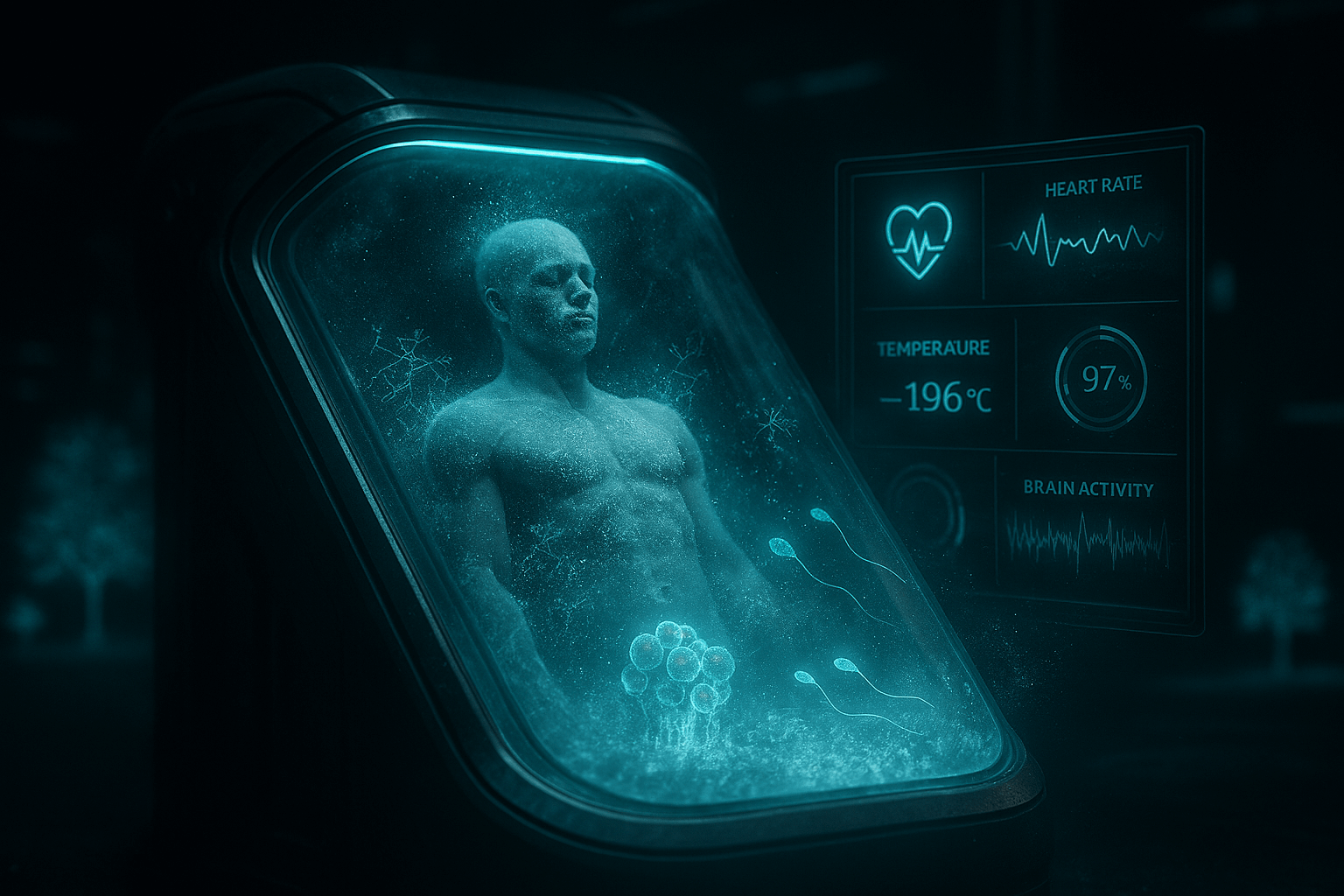
The probe picks up a chilling signal from the edge of life: a trauma victim, blood draining away, heart silenced, body cooled to the brink—yet not gone, merely suspended in time. What happens when death is put on hold, granting surgeons hours to mend the unmendable?
Scanning deeper: EPR—Emergency Preservation and Resuscitation—is transforming emergency medicine, inducing reversible stasis to rescue those on the verge of irreversible loss.
How It Actually Works
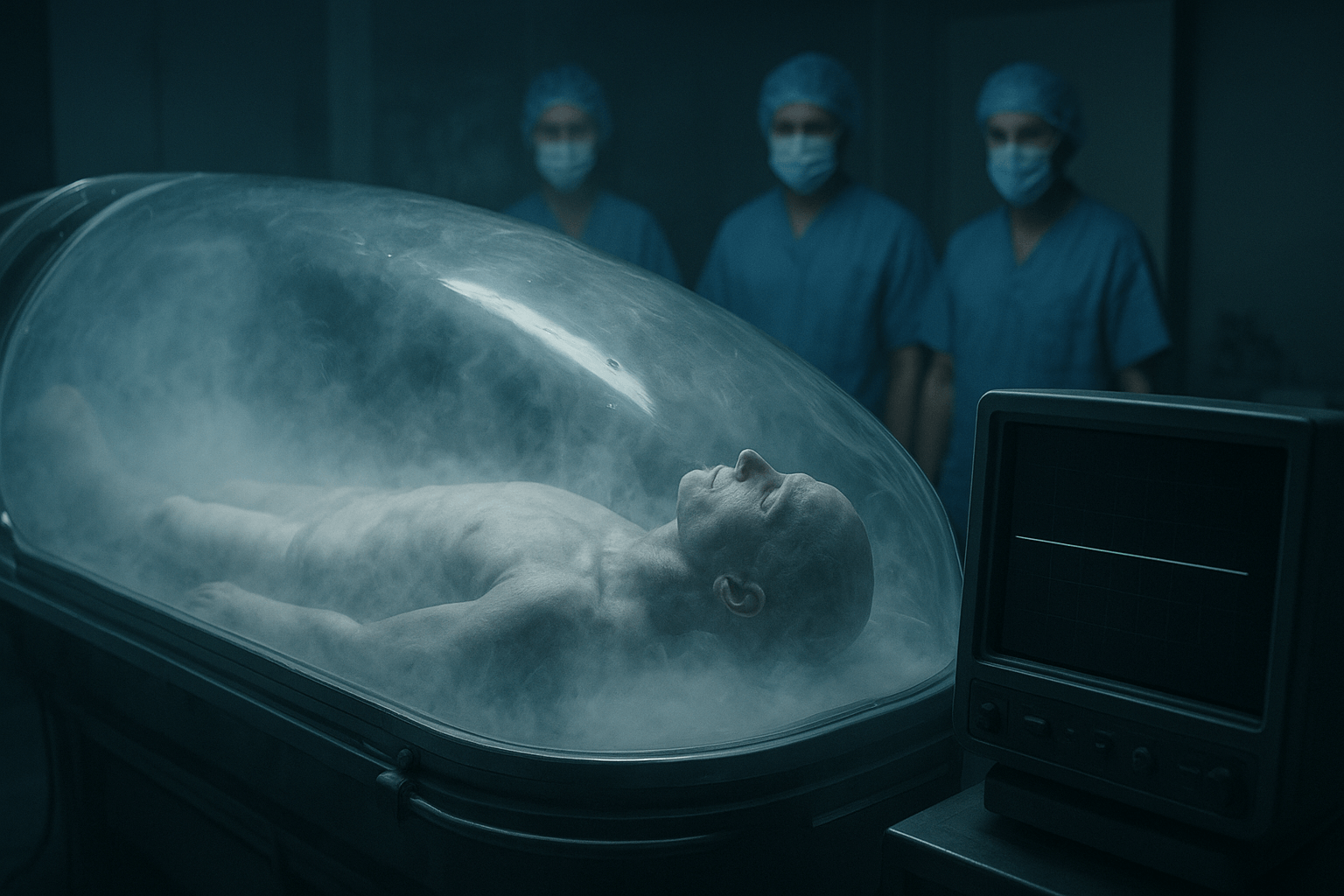
EPR is a high-stakes battle against cellular collapse. In severe trauma—gunshots, stabbings, aortic ruptures—blood loss outpaces repair. Brain cells perish after 5 minutes without oxygen. EPR extends that window to up to 2 hours.
The process is stark, precise, and fully reversible.
What Doctors Do — Step by Step
- Cardiac arrest confirmed — no pulse, no chance with standard CPR;
- Rapid cannulation — large tubes inserted into femoral artery and vein;
- Blood drained — 4–6 liters removed in under 3 minutes;
- Ice-cold saline (4–10°C) pumped in via modified ECMO circuit;
- Core temperature drops to 10°C in 15 minutes — EEG goes flat;
- Surgeons repair injuries in a bloodless field — no bleeding, perfect visibility;
- Gradual rewarming — oxygenated blood reintroduced at 0.5°C per minute;
- Heart restarted with defibrillation — patient returns to life.
But Isn’t That Death?
Yes — and no.
At 10°C:
- Heart: stopped
- Brain: no electrical activity
- Metabolism: reduced by 90%
- Cellular damage: nearly halted
Researchers term it “induced torpor” or biological stasis—echoing hibernation in animals surviving harsh winters. The body isn’t struggling; it’s simply paused.
Real Trials — Real Lives Saved
The EPR initiative launched at UPMC Presbyterian Hospital, Pittsburgh, led by Dr. Samuel Tisherman. Initial human trial: 2019. Criteria: only cases with <5% survival odds and penetrating trauma.
By 2024, over 20 patients have undergone EPR. While full results await publication:
- Survival rate: ~40% — vs. expected 0–7% with standard care;
- Neurological outcomes: 70% of survivors regained full cognitive function;
- Longest stasis: 1 hour 47 minutes at 10.2°C.
“We literally bought them time. It’s like pressing the pause button on death.” — Dr. Samuel Tisherman, EPR pioneer
Why It Works: The Science of Cold
Each 10°C temperature drop halves metabolic rate (Q10 rule). At 10°C:
- Oxygen demand: 1/8th of normal
- Brain glucose use: reduced 12-fold
- Ischemic tolerance: extended from 5 min to 120 min
It’s not true freezing—it’s super-cooled hibernation.
Risks — Because It’s Not Magic
- Coagulopathy: Cold blood doesn’t clot — bleeding can restart during rewarming;
- Reperfusion injury: Sudden oxygen return can trigger inflammation storms;
- Brain edema: 12% of patients develop swelling requiring decompression;
- Ethical line: When do you stop? 1 hour? 3? A day?
What’s Next
- 2026: FDA fast-track approval for Level I trauma centers;
- 2028: Portable EPR units for ambulances and battlefields;
- 2030s: Elective “therapeutic torpor” for stroke, heart attack, or complex brain surgery;
- Space medicine: NASA funds EPR research for Mars missions — astronauts in stasis for 6-month transit.
Key signal: death may evolve from an instant to a negotiable interval.
“We don’t yet know how to defeat death. But now we can — put it on pause.”
The probe emerges from the chilled stasis and fades into shadow: life’s fragile thread now has a pause button.